Scientists paint a picture of how ECMO alters the effectiveness of antibiotics in a world first
A network of international researchers have documented how extracorporeal membrane oxygenation (ECMO), the life-saving blood oxygen therapy, changes the dosing requirements of antibiotics in critically ill patients, in a study that is set to change the way ECMO is used and administered and improve outcomes for the health system’s sickest patients.
“This global research initiative began by observing just one patient in the Adult Intensive Care Unit,” said Associate Professor Kiran Shekar, Senior Intensive Care Specialist, The Prince Charles Hospital (TPCH) and Research Fellow at The University of Queensland.
“Professor John Fraser and I watched as the sedated patient began to wake up as ECMO was initiated, and suspected this was due to some of the sedative agent being adsorbed by the ECMO membrane. We hypothesised that if the sedative was being adsorbed, then perhaps so were the lifesaving antibiotics and antivirals the patient was receiving, however there were no immediate signs of this in the same way we could see the sedation being adsorbed.
“This led us to run some preclinical models of ECMO where we could demonstrate that multiple drugs were being adsorbed out of the blood. We translated preclinical findings into an international clinical study that has the potential to change the way antibiotics and antivirals are administered and monitored in the most critically ill patients.”
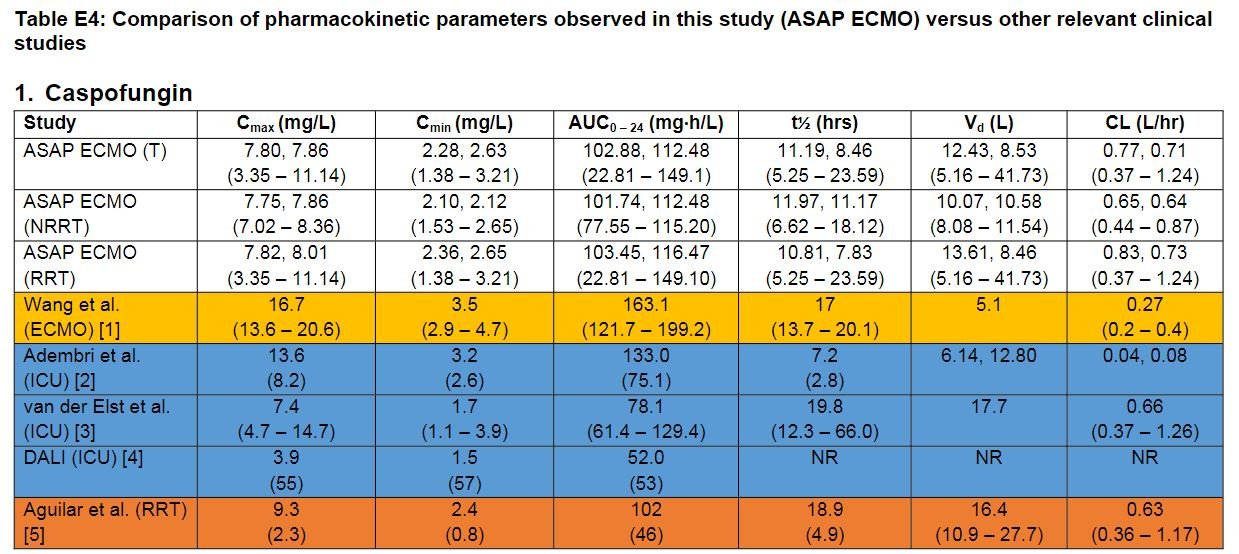
Professor Jason Roberts, Acting Director of The University of Queensland Centre for Clinical Research (UQCCR), who designed the project with Professor John Fraser, Founder of TPCH’s Critical Care Research Group (CCRG), and Associate Professor Kiran Shekar, said that the ‘ASAP ECMO’ study, just published by the Journal of The American Thoracic Society (ATS), is both the first multinational and the largest study to describe the pharmacokinetics of multiple antimicrobials in ECMO patients.
“Seeded from a clinical problem, we took a holistic and global approach to gather robust clinical data to understand how to effectively dose critically ill patients, an area where data was previously lacking.
“Working with great minds across Australia, New Zealand, South Korea and Switzerland, our primary aim was to record how ECMO patients reacted to antibiotics for the duration of their treatment period, and to examine if current regimes and standards were sufficient.
“We included 993 blood samples from 85 patients, and found that approximately 40 percent of profiles analysed did not achieve the desired concentration levels of antibiotics.
“From a science point of view, our work from bench to bedside has resolved many of the uncertainties around antimicrobial, sedative and analgesic drug dosing in ECMO patients, and I am confident it will make a difference to the lives of our patients and their families, but also to the confidence that intensive care clinicians have with their drug and dosing choices” said Professor Roberts.
“The study would not have been possible without the persistence of Associate Professor Kiran Shekar, the firm support of Professor Jason Roberts, our extended ECMOnet family, the NHMRC’s CRE ACTIONS and CRE RESPOND, and our patients. I would also like to recognise Dr Hafiz Abdul-Aziz who provided strong leadership in the finalisation of the projects.
“But most importantly we need to acknowledge the many men and women who worked tirelessly to screen and recruit patients. The labour required to collect and label close to 1000 samples cannot be overlooked, and for that I am truly grateful,” said Professor Fraser.
Associate Professor Kiran Shekar echoed this gratitude for the cohort of international collaborators for their valuable contributions to the game-changing project.
“What started as a fleeting idea between friends, rapidly grew to a fully-fledged international research project brought to logistical conclusion by Professor Fraser, Professor Roberts, Dr Abdul-Aziz and their extensive international networks. Breaking down barriers for a truly silo-free research and knowledge ecology, I am positive we will do more work in this area and look forward to many more important collaborations.”
More information
-
Professor John F Fraser is Founder and Director of the Critical Care Research Group (CCRG), The Prince Charles Hospital & University of Queensland; Director of ICU St Andrew’s War Memorial Hospital; President Asia-Pac Extracorporeal Life Support Org; Founding member of the global clinical trials ECMOnet & CoChair Queensland Cardiovascular Research Network.
-
Professor Jason Roberts is Director, CRE RESPOND, Acting Director, UQ Centre for Clinical Research, NHMRC Leadership Fellow, The University of Queensland, Interim Diector Herston Infectious Diseases Institute (HeIDI), and Pharmacist Consultant, Royal Brisbane & Women’s Hospital.
-
Established in 2004 by Professor John Fraser, , CCRG is Australia’s largest multi-disciplinary critical care research facility with 80+ world-leading clinicians, engineers, scientists, economists, and support staff from 6 continents. Under his leadership, CCRG has created 7 purpose-built biology, engineering, bio-fabrication labs and the largest preclinical ICU in the southern hemisphere.
-
Centre of Research Excellence RESPOND – Reduce the burden of antimicrobial resistance through optimal, personalised dosing.
CRE RESPOND is led by Professor Jason Roberts and is a $2.5 million multi-institutional collaborative funded by the National Health and Medical Research Council of Australia from 2021-2026 to reduce the burden of antimicrobial resistance through optimal personalised dosing. It extends upon its predecessor, CRE REDUCE (2016-20). It aims to bring about new findings from research and share these with clinicians so that they can provide better treatment to their patients and improve outcomes for them and their families.
-
CCRG was awarded a key grant from the National Health and Medical Research Council in 2014 to establish the Centre of Research Excellence (CRE) in Advanced Cardio-respiratory Therapies Improving Organ Support (ACTIONS). CRE ACTIONS is a unique, global level collaboration of clinical, engineering and scientific experts in Ventricular Assist Devices (VAD) and Extracorporeal Membrane Oxygenation (ECMO) who together with patients supported by these therapies, is addressing the range of key challenges associated with the clinical implementation of these technologies, to accelerate the translation of knowledge from the laboratory to the bedside.
-
A/Professor Shekar is a Senior Intensive Care Specialist, Adult Intensive Care Service at the Prince Charles Hospital. He holds academic appointments as Associate Professor at the University of Queensland, Adjunct Porfessor at Queensland University of Technology and Associate Professor at Bond University, Gold Coast. Shekar is the recipient of the Metro North Health Clinician Research Fellowship. Shekar specialises in design and conduct of both pre-clincial and clinical studies. His ongoing research programs bring together clinicians, multidisciplinary allied health professionals, engineers, scientists, health economists, industry and policy experts to minimise the burden of invasive mechanical ventilation in intensive care units and to improve access to intensive care services around the world.
-
Dr Hafiz Abdul–Aziz is currently a research fellow at the Burns, Trauma and Critical Care Research Centre (BTCCRC) and Centre for Research Excellence for Redefining Antimicrobial Use to Reduce Resistance (CRE REDUCE) at the University of Queensland, Australia. Hafiz is a clinical pharmacist with a strong interest in clinical research, particularly those involving multi-centre and multi-national collaborations.