Heart transplant gamechanger opens possibility of global transport
The Sunday Mail, 25 August 2024, by Jackie Sinnerton.
Miles Government announces $1.6m funding to allow CCRG to continue our life-saving and practice-changing research.
World-leading Australian scientists have developed miracle technology to keep human hearts alive for 12 hours outside the body. They’re now aiming for 48 hours.
Lifesaving transplant hearts would be flown across the globe as Queensland researchers set out to extend the life of organs to 48 hours.
The Critical Care Research Group at Brisbane’s Prince Charles Hospital can already keep a donated heart viable for a flight from Tasmania to Perth using the revolutionary hypothermic oxygenated perfusion (HOPE) technology, but their new “48 hour study” is offering hope there will be no geographical barrier to matching a patient with a heart.
HOPE is the greatest innovation in heart transplant surgery and has garnered interest from surgeons across the world. There is great hope the science will also be applied to lungs and kidneys.
Preclinical trials in the use of the technology, initiated by Swedish professor Stig Steen, were carried out in Brisbane with great success, outshining the “ice in an Esky” method of organ transportation which allows the heart to remain “ex vivo”, or outside the body, for four hours before the heart muscle starts to deteriorate.
“We are now confident that we can keep the heart outside the body in good condition for 12 hours and now we are looking to do more. We know from our trials that hypothermic oxygenated perfusion works and works well,” John Fraser, director of the Critical Care Research Group at PCH, said.
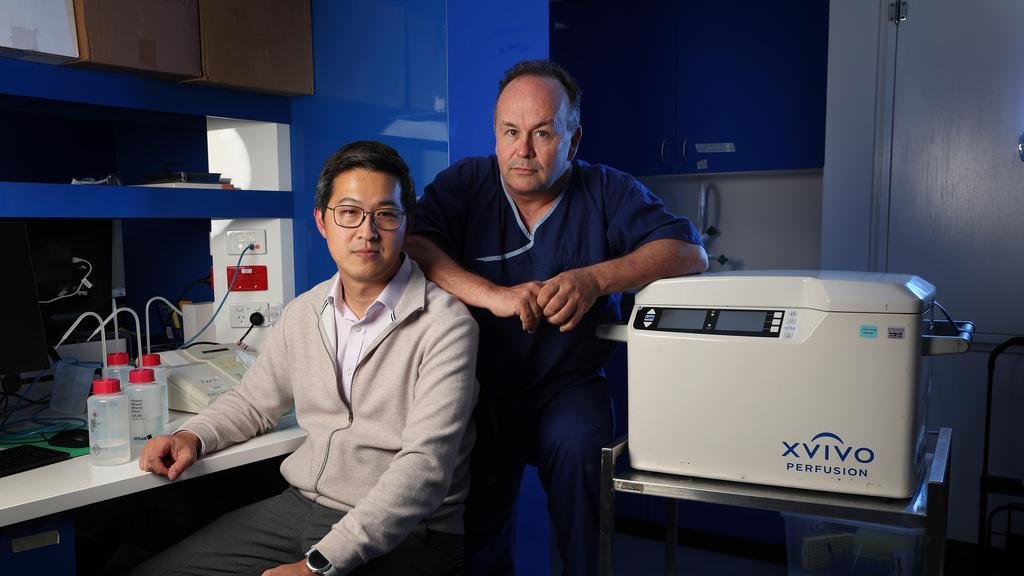
CCRG's Dr Jacky Suen, STARLab lead, and Prof John Fraser with the hypothermic oxygenated perfusion (HOPE) rig that has saved the lives of 100 people and counting. Photo: Liam Kidston / The Courier Mail
Queensland's Health Minister Hon Shannon Fentiman (left) with CCRG researchers including Prof John Fraser recognise the 100th heart transplanted using the HOPE perfusion rig.
“Our research is leading national and international clinical trials and setting new clinical guidelines to help make sure every heart that’s donated has the best chance of being transplanted to a patient.
“This is something we want to do not only for recipients but to fulfil the wish of the donors who wanted to give an organ. It is an amazing gift for a person and their family to agree to donate at organ.”
Only one in five donor hearts can be transplanted due in part to the logistics of transporting organs. The world-changing HOPE technology will help stop organs going to waste. It is a device that uses a “medical Gatorade” which has a mix of vitamins and chemicals to keep the organ “alive”.
The government is boosting the important medical research with a $1.6m grant to the Critical Care Research Group.
“One day we would love to see this device used across the world as standard,” Professor Fraser said. “I don’t know if it will replace the ice in Esky as that has it’s place for short transport cases, but the world’s scientists and transplant doctors have their eyes on Queensland.
The Critical Care Research Group celebrates its 20-year anniversary this year.
Health Minister Shannon Fentiman said the HOPE technology had saved the lives of 100 people so far.
“This research will no doubt save thousands more as it rolls out across the globe to become standard clinical practice,” she said. “Supporting medical innovation and research is so important and something that the Miles government is dedicated to – which is why we are pleased to also announce this funding for the Critical Care Research Group.
“As a proud organ donor myself, I truly believe that organ donation is one of the greatest gifts you can give and this research means every organ donated has the best chance of reaching a patient.”
For the first time, Queenslanders can be prompted to register as an organ donor when they renew their driver's licence or vehicle registration, in a bid to increase the state’s share of donors.
Kate Phillips (left), pictured with former CCRG Research Fellow, Dr Louise See Hoe, and heart transplant recipient Alex Moroianu, who received her new heart via through CCRG's Living Heart Project. Pictured at CCRG's 20-year anniversary dinner 18 July 2024.
Living proof of donor success
At age 27, Kate Phillips was one of the lucky ones.
When her life was hanging on a knife edge, she received the gift of a heart and double lung transplant.
“I am so very aware of how many things have to align for suitable organs to become available for transplant and I will be forever grateful that people at the most tragic time of their lives choose to give the gift of life,” Ms Phillips, now 39, said.
“When you live with transplanted organs you approach life day by day. Taking medications to keep everything functioning is a constant balancing act. I don’t know if I will need another transplant in the future but knowing that there are so many medical advancements gives me comfort,” she said.
Ms Phillips, who has been a patient at Prince Charles Hospital since she was an infant, was the first female transplant recipient to compete in an Australian ironman event.
She was born with heart disease and pulmonary hypertension.
This article originally appeared in The Sunday Mail 25 August 2024.